

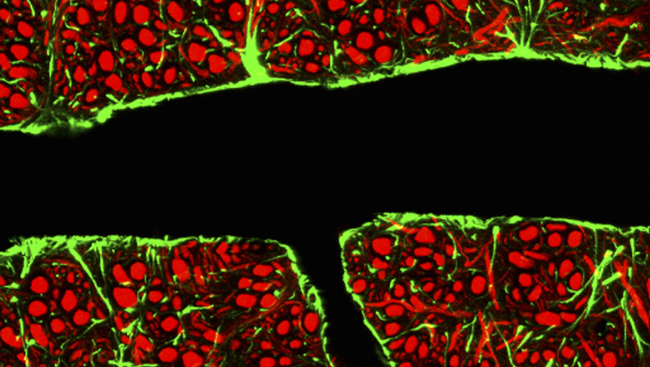
The turnover of FAK has been shown to regulate barrier function, and dysregulation of FAK impacts the integrity of cellular barriers ( Ivey et al., 2009) by increasing paracellular permeability, which can imply disruption of the barrier function ( Ma et al., 2013). Focal adhesion kinase (FAK), also named protein tyrosine kinase 2 (PTK2), regulates signaling pathways involved in cell-cell adhesion and focal adhesion complexes in endothelial cells ( Lee et al., 2010 Siu et al., 2009). This restricts the paracellular flux of hydrophilic molecules and regulates the migration of cells across the endothelial barrier ( Alon and van Buul, 2017). Intercellular tight junction (TJ) proteins seal the spaces between adjacent endothelial cells and separate the apical from the basolateral side. Basal lamina, astrocyte ‘end-feet’ and pericytes also contribute to restrict permeability ( Daneman and Prat, 2015 Armulik et al., 2010). The microvascular lumen is covered by highly specialized endothelial cells characterized by low permeability, low pinocytic activity and high transcellular electrical resistance (TCER) ( Stamatovic et al., 2008). The BBB is anatomically localized to the cerebral microvasculature, which is constituted by capillaries with a luminal diameter (Ø) of <10 μm, arterioles and venules (~10–100 μm Ø) ( Wilhelm et al., 2016 Gould et al., 2017). Of these, the BBB exerts the greatest immediate impact on the cerebral microenvironment. Three main cellular barrier systems protect neurons from blood-borne external insults, such as infection: the blood-brain barrier (BBB), the blood-cerebrospinal fluid barriers and the meningeal barriers ( Coureuil et al., 2017). The vertebrate central nervous system (CNS) is protected by restrictive cellular barriers that maintain homeostasis and regulate passage of molecules and cells to the brain parenchyma ( Abbott et al., 2006). The integrity of the microvascular BBB restricts parasite transit, which conversely is exacerbated by the inflammatory response. gondii to the central nervous system occurs principally across cortical capillaries. The data reveal that the initial passage of T. Finally, pharmacological inhibition or Cre/ loxP conditional knockout of endothelial focal adhesion kinase (FAK), a BBB intercellular junction regulator, facilitated parasite translocation to the brain parenchyma. Pro- and anti-inflammatory treatments of mice with LPS and hydrocortisone, respectively, impacted BBB permeability and parasite loads in the brain parenchyma. gondii triggered inflammatory responses in cortical microvessels and endothelium. However, sparse focalized permeability elevations were detected adjacently to replicative parasite foci. Early invasion to the parenchyma (days 1-5) occurred in absence of a measurable increase in blood-brain barrier (BBB) permeability, perivascular leukocyte cuffs or hemorrhage. Shortly after inoculation in mice, parasites mainly localized to cortical capillaries, in preference over post-capillary venules, cortical arterioles or meningeal and choroidal vessels.
Here, we addressed the role of the cerebral vasculature in the passage of T. Yet, the single-celled parasite Toxoplasma gondii commonly causes latent cerebral infection in humans and other vertebrates. The cellular barriers of the central nervous system proficiently protect the brain parenchyma from infectious insults.


 0 kommentar(er)
0 kommentar(er)
